3 orders of MLTC systems science¶
Objective¶
In our initial development phase meetings, in became evident that there was prima facie overlap between different contributing disciplines. For example, participatory design (PD) articulates methods and theory for involving stakeholders in the co-production of artefacts and systems; PD has it's origins in the Scandinavian trade union movement of the early 1970s and then later, was adopted in software engineering and human computer interaction. In healthcare, the patient and public involvement (PPI) agenda traces it's origins back to a similar historical period, coinciding with civil rights movements and represents a correction to the traditional model of medical research being dominated by professional agendas. In the cognate literature on design, we find similar historical and theoretical overlap in these diverse fields' appeals to concepts in systems theory (that in turn, can also be found in the systems engineering literature).
In this work package, we attempted to pull together and organise examples from the literature that situate system engineering for healthcare (for example, the Engineering Better Care report) in the broader context of design methods, learning health systems and systems science more generally.
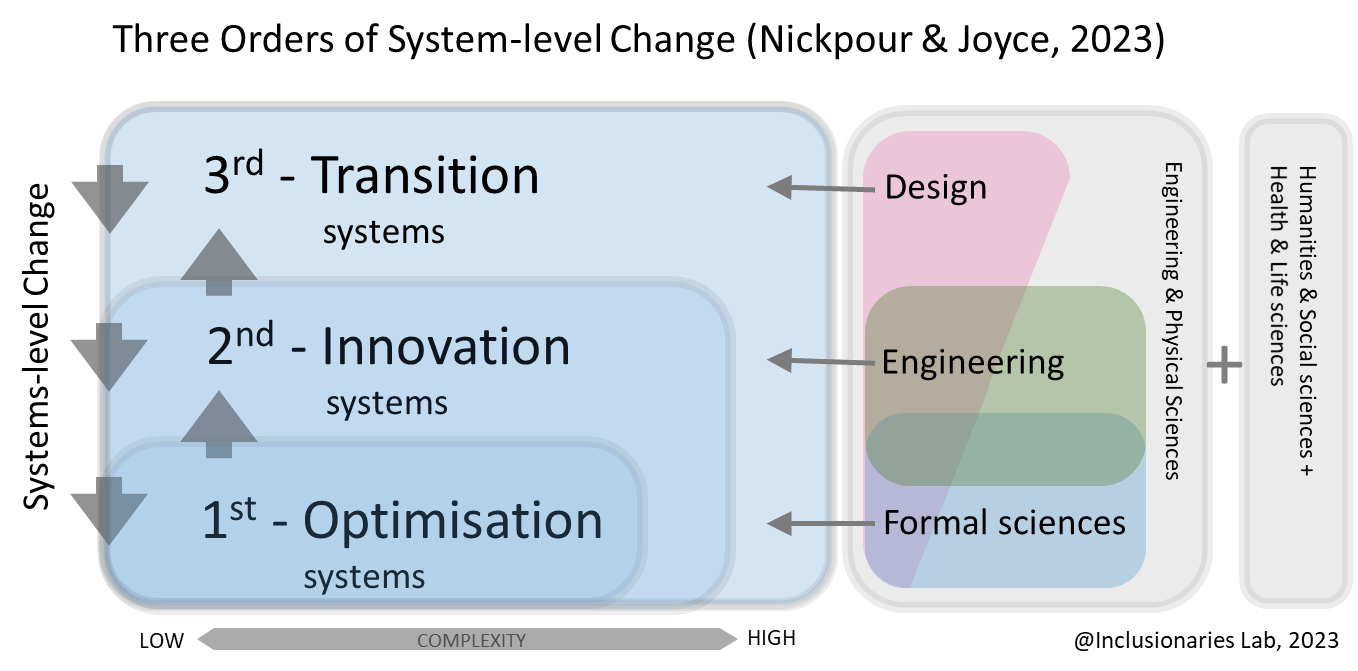
We wanted to articulate a framework to show how system theory or "systems thinking" can be leveraged for different problems in healthcare that we expect systems engineering to help improve -- for example, improving patient journeys by modelling and understanding how systems work currently and exposing opportunities for improving them. We postulated that methods from different branches of systems, formal and engineering sciences might be more useful and applicable for different parts of modern, complex healthcare systems.
3 orders of MLTC systems science¶
Our cooperative of disciplines includes systems modelling, systems engineering, systemic design, clinical research, public health research, and health and care commissioning and provision.
We apply three orders of systems science to health & care systems, distinguished by: a) how they define a system;
b) the associated research methods; and c) the tools, frameworks and techniques.
1) 1st-Order: Optimisation optimises discrete components with clear boundaries, quantified inputs/outputs, crude ontologies and a governing process with feedback and error correction. For example, feedback to GPs on their potentially harmful prescribing of antipsychotics and interacting drugs with no wider context.
2) 2nd-Order: Innovation is the mainstay of systems engineering in healthcare. Modelling is ontological, but tolerates ill-defined boundaries, uncertainty and unknowns, and may adopt simulation methods, or statistical process control. For example, modelling the potential impacts of a weight management clinic/service for people taking antipsychotic medication, after psychotic symptoms are controlled.
3) 3rd-Order: Transition extends to soft systems with porous boundaries, nonlinear behaviours, and contextual sensitivity. Key approaches are participatory; Patient and public engagement and involvement (PPIE) with practitioner co-design, action research, systemic design, and transition design. This approach suits transitioning from single condition/pathway/service optimisation to integrated MLTC approaches. For example, transitioning from NHS weight-management referral to a package of wider cardiovascular risk reduction and social support/prescribing for people taking antipsychotic medication.